For individuals with opioid use disorder, an additional substance use disorder is associated with increased mortality risk
Opioid use is a significant contributor to premature death, including drug-related poisonings and suicide. While research and monitoring data have clarified the impact of opioids on mortality risk, approximately 50-75% of those with opioid use disorder meet criteria for another substance use disorder. To increase the representativeness of practice and policy recommendations, this study took a critical look at opioid-related mortality among opioid use disorder patients with and without co-occurring substance use disorders.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Opioid-related deaths remain significant public and individual health concerns in the United States. While a considerable amount of research focuses on the role of opioid use in fueling opioid- and other drug-related deaths, surprisingly little effort has been devoted to examining mortality risk among individuals who also use other substances, or who have co-occurring substance use disorders.
Polysubstance use – the use of multiple substances in general or in combination – is very common (e.g., approximately 50-75%) and is associated with significant risk for negative health outcomes and can exacerbate mortality risk. Other central nervous system depressants, like benzodiazepines, alcohol, or other synthetic opioids are especially dangerous in combination with opioid drugs, with research increasingly demonstrating the harms associated with co-use of opioids and stimulant drugs (e.g., cocaine).
Opioid-related deaths are often classified as overdose-related suicides, raising the concern that individuals with opioid use disorder and other co-occurring substance use disorders may be at increased risk for suicide mortality. Documentation of the rates of mortality and other adverse outcomes among individuals who engage in polysubstance use could be beneficial. These researchers used a large Medicaid claims database to compare opioid-related mortality and suicide risk for patients with opioid use disorder alone relative to those with and co-occurring opioid and other substance use disorders.
HOW WAS THIS STUDY CONDUCTED?
The researchers conducted a retrospective medical claims study, using IBM Watson Health MarketScan Medicaid enrollment/claims data. The patients selected from this data set for this analysis included non-Medicare-eligible individuals, between 18 and 65, enrolled in Medicaid between 2016-2017, and had a primary opioid use disorder diagnosis attached to at least one Medicaid claim in 2016. For their analysis, the researchers identified eligible patients in their Medicaid database from 2016, the examined outcomes of these individuals in calendar year 2017. They were specifically interested in examining whether patients with opioid and other co-occurring substance use disorders had higher risk of negative outcomes vs. patients with opioid use disorder alone.
For the current study, the researchers examined negative outcomes of all-cause mortality (i.e., death for any reason), opioid-related poisoning (e.g., opioid-involved overdose), suicidal ideation, and opioid prescription fills that were not associated with medication for opioid use disorder treatment (i.e., not MOUD such as buprenorphine or methadone). To identify patient diagnoses, the researchers used clinician-entered diagnosis codes (International Classification of Diseases, Tenth Revision, Clinical Modification; ICD-10-CM) for opioid use disorder; alcohol use disorder; cannabis use disorder; sedative, hypnotic, or anxiolytic use disorder; cocaine use disorder; other stimulant use disorders (e.g., methamphetamine); hallucinogen use disorder; inhalant use disorder (inhalant and hallucinogen use disorders were later grouped into an “other substance use disorder” category); and unidentified substance use disorder. Individuals who met criteria for an opioid use disorder and one or more of the other substance use disorder categories were considered to have co-occurring substance use disorders.
The researchers also included cases where the substance of use was noted as a concern but that might not have met criteria for a substance use disorder, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Lastly, the researchers retrieved and examined individual-level predictors of negative outcomes in 2017, such as age, sex, race, health care plan type, urban vs. rural status, presence vs. absence of nicotine use disorder, and other non-substance related psychiatric diagnoses. These psychiatric diagnoses included anxiety (other than posttraumatic stress disorder), posttraumatic stress disorder, attention-deficit hyperactivity disorder, depressive disorder, schizophrenia, bipolar disorder, and “other” mental health disorders.
Participants in the study included 58,748 Medicaid enrollees with OUD from 2016. The age range was 18-64 and almost two-thirds of enrollees were women (61.7%). White race (78.8%) was the most common, followed by Black (10.3%), unspecified (8.9%), Hispanic (1.1%), American Indian/Alaska Native (.6%), Asian/Native Hawaiian/Pacific Islander (.2%), and other (.1%). Psychiatric diagnoses were also common (64.5%), including anxiety (44.6%), depression (40.3%), bipolar disorder (17.5%), posttraumatic stress disorder (10.1%), other diagnoses (9.7%), attention-deficit hyperactivity disorder (6.5%), and schizophrenia and other psychotic disorders (6.0%). A total of 23.9% had a co-occurring substance use disorder, including alcohol (7.7%), cannabis (3.7%), cocaine (3.4%), other stimulants (2.7%), sedative/hypnotic/anxiolytics (1.4%), hallucinogens (.1%), inhalants (.2%), or other/unidentified substance use disorder (11%).
WHAT DID THIS STUDY FIND?
Adverse events and mortality risk.
Compared to individuals with opioid use disorder alone, individuals with a co-occurring substance use disorder were 48% more likely to experience opioid-related poisoning, 76% more likely to experience an all-cause poisoning event, and 80% more likely to experience suicidal ideation in 2017. There were no differences between these individuals regarding rates of opioid prescriptions in 2017.
Figure 1.
Subgroup analyses for co-occurring substance use disorder groups.
Particular patterns emerged when the researchers examined combinations of co-occurring substance use disorders. For example, individuals with opioid and cocaine use disorders were the most likely to experience all-cause or opioid-related poisonings and evidenced the highest risk for suicidal ideation. As displayed in the figure below, the presence of any co-occurring substance use disorder was associated with elevated risk of negative outcomes in 2017, with some exceptions regarding opioid use-related poisonings and opioid prescriptions.
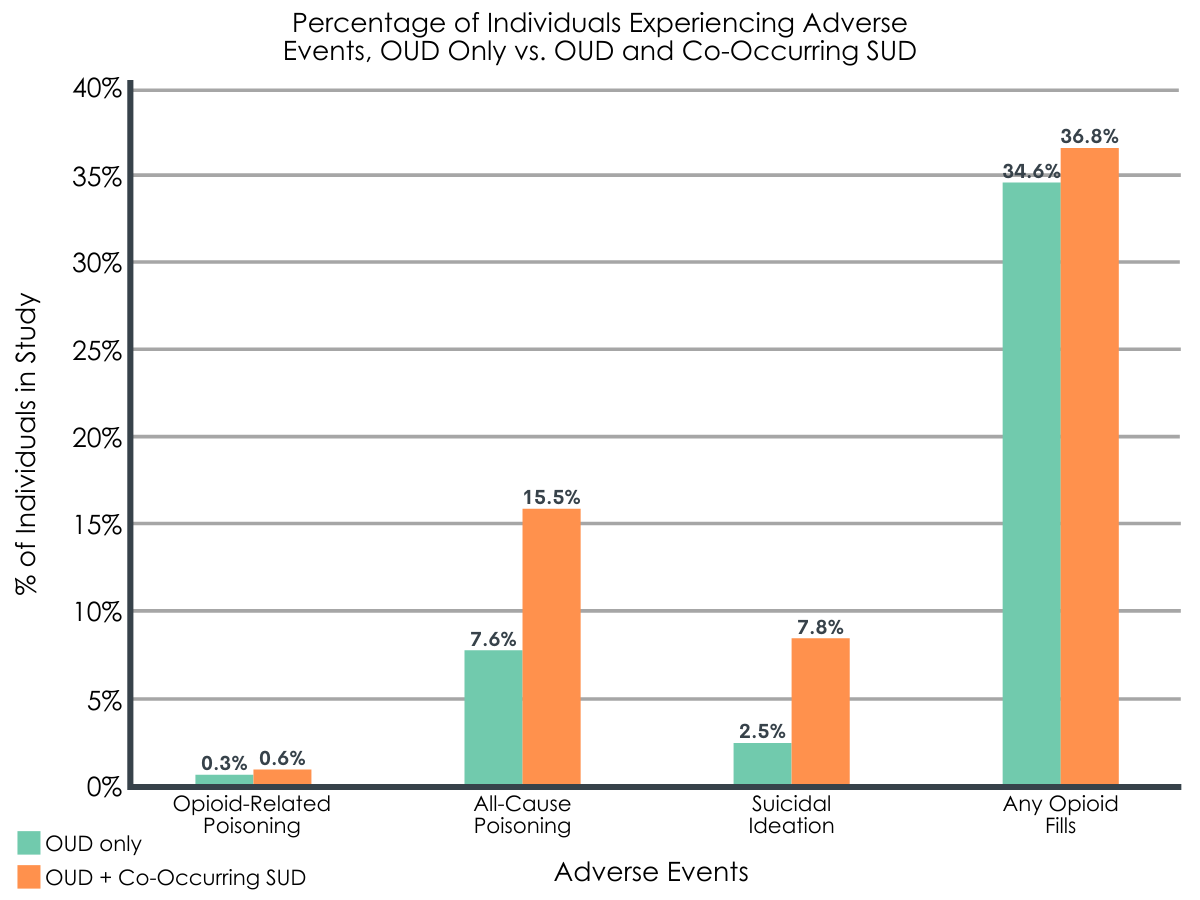
Figure 2.
The researchers also found that patients with co-occurring substance use disorders were more likely than those with opioid use disorder alone to be younger, male, non-White, and also evidenced higher rates of other psychiatric diagnoses (e.g., depression, posttraumatic stress disorder).
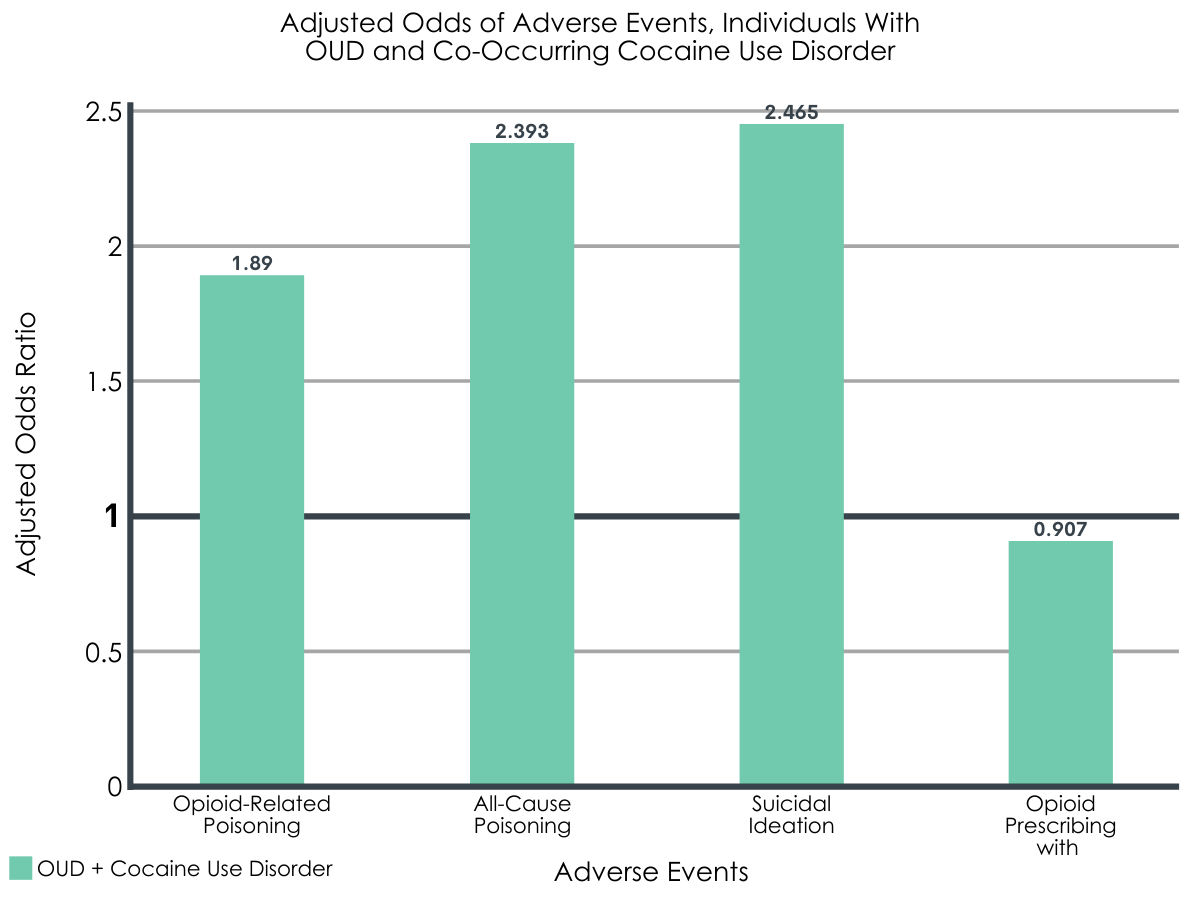
Figure 3. The researchers used odds ratios (ORs), which here indicate the odds of adverse events occurring. An OR of more than 1 indicates that event is more likely to occur compared to the control or comparison condition (e.g., OR of 2 = 2x more likely to occur). An OR of less than 1 indicates that event is less likely to occur (e.g., OR of 0.5 = 1/2 as likely to occur).
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
In this study, the researchers used diagnoses and Medicaid claims data from 2016 to examine predictors of all-cause mortality, opioid-related poisoning, suicidal ideation, and opioid prescription fills among patient with opioid use disorder in 2017. The researchers found that in most cases, the co-occurrence of opioid use disorder with another substance use disorder was associated with higher risk of negative outcomes. Patients with opioid and cocaine use disorder were at greatest risk – they evidenced the highest rates of all-cause mortality, opioid-related poisoning, suicidal ideation.
The outcomes among individuals with an opioid use disorder and any co-occurring substance use disorder were generally worse. These findings might reflect overall severity of substance use disorder and impairment, with individuals using more substances and meeting criteria for multiple substance use disorders also being more likely to engage in high-risk substance use, leading to mortality. This study also highlights the possible and relative impacts of certain patterns of co-occurrence, and specifically spotlights risks associated with co-occurring opioid and cocaine use disorders. The combination of opioid and cocaine use disorder might suggest that these patients are more likely to co-use cocaine and opioids, which can be a deadly combination that is also on the rise. Use of a stimulant such as cocaine, for example, can result in the perception of a diminished sedative effect from opioid use effect leading to higher dosing of opioids increasing risk of overdose and mortality.
Despite these known opposing pharmacological effects, however, the risk of opioid-specific overdose death for cocaine and opioid co-use was less pronounced than it was for all-cause mortality suggesting alternative explanations. Another possibility, for example, could relate to increasing rates of contamination of cocaine with synthetic opioids such as fentanyl. Finally, aligning with other research on polysubstance use and mental health, individuals with co-occurring opioid and other substance use disorders were also more likely than those with opioid use disorder alone to be diagnosed with a psychiatric disorder.
It is possible individuals with psychiatric disorders, especially more severe variants, are at risk for using multiple substances in an effort to cope with extreme distress; alternatively, greater use of more substances may be inducing more brain changes that can result in greater negative neuropsychiatric effects and related psychiatric symptoms. Best practices for individuals with severe psychiatric disorders might attend to this risk for co-occurring opioid and other substance use disorder, and, in turn, the increased risk for negative outcomes association with these co-occurring disorders.
- LIMITATIONS
-
- Authors identified patients with opioid use disorder-related claims in 2016 and evaluated adverse outcomes recorded in 2017. This follow-up period limits analysis of adverse events that might have also occurred in 2016, or after 2017.
- The researchers did not discuss or account for the possibility of positive detection bias within the Medicaid database. Positive detection bias is an artifact of patients with more severe disorders or healthcare need also having more complete medical data, relative to patients who are less severe and how might have missing data on fields more likely to be filled among the former. This could have also resulted in incomplete or less consistent diagnostic information for some patients, and possible misclassification of patients within diagnostic groups.
- The researchers did not account for combinations of more than one substance non-opioid-related disorder in combination with opioid use disorder (e.g., 3 or more substance use disorders).
- Suicide ideation vs. attempt data is limited in large claims databases, and often undercounted. Suicide attempts vs. accidental overdoses can also be misclassified.
- The scope of this analysis is limited to non-Medicare-eligible Medicaid recipients. These data also do not include individuals with other forms of commercial insurance.
- The researchers allude to the fact that not all states were represented in their Medicaid claims database but do not specify which. This limits inferences regarding unrepresented states or geographic areas.
BOTTOM LINE
Medicaid patients identified as having an opioid use disorder in 2016 were followed to examine negative outcomes and also predictors of these outcomes in 2017. Compared to patients with opioid use disorder alone, those with opioid and another substance use disorder were generally more likely to experience negative outcomes in 2017, including all-cause mortality, opioid-related poisoning, suicidal ideation, and opioid prescription fills. The group with the highest odds of all-cause mortality, opioid-related poisoning, and suicidal ideation in 2017 were patients with co-occurring opioid and cocaine use disorder.
- For individuals and families seeking recovery: Use of opioids and other drugs, especially in combination, can be more deadly than the use of opioids alone. These researchers found that individuals with any combination of opioid and non-opioid disorder were more likely to experience negative outcomes over time, especially opioid-related poisoning, suicidal ideation, and all-cause mortality. Individuals with the combination of opioid and cocaine use disorders were the most likely to experience negative outcomes. With respect to the slightly more pronounced opioid-related poisoning deaths with cocaine co-use, this finding could reflect the risks associated with using opioids and cocaine together, which could stem from the stimulating effects of cocaine use offsetting some of the sedating effects of opioids, prompting increasing and potentially more lethal consumption of doses of opioids. It could also be attributable to possible contamination of cocaine with synthetic opioids such as fentanyl. Unfortunately, it is very challenging or impossible for drug users to identify when cocaine (or heroin) has been contaminated with more potent fentanyl before it is too late. For individuals and families, it is also worth noting the fact that suicidal ideation was elevated among individuals with opioid use disorder and other co-occurring substance use disorders. Discussing or sharing these concerns with loved ones can be lifesaving.
- For treatment professionals and treatment systems: The results of this study provide further support for the benefits of screening patients for all types of substance use, as well as particular use patterns to assess relative risk. For example, patients who ingest opioids through smoking vs. intravenous use will have lower vs. higher risk for death, respectively. Patients who use drugs in certain combinations, such as combining central nervous system depressants (e.g., opioids and alcohol) or combining opioids with stimulants (e.g., cocaine) evidence considerably higher risk for drug-related poisonings and death. Assessing these risk factors can be lifesaving and also help providers link patients to appropriate care and services. Lastly, the finding that individuals with opioid and co-occurring substance use disorders evidenced higher levels of psychiatric disorder as well as suicidal ideation suggest that enhanced suicide screening, prevention, and intervention is warranted with these patients.
- For scientists: Few studies have examined the relative risk for all-cause mortality, opioid-related poisoning, suicidal ideation, and opioid prescription fills among patients with opioid and co-occurring substance use disorders. Future research may benefit from examination of additional combinations of disorders, such as co-occurrence of other psychiatric diagnoses (e.g., PTSD), and additional combinations of co-occurring substance use disorder (e.g., more than 2 co-occurring disorders). This study was also limited by the examination of diagnostic status in 2016 with negative outcomes recorded for these patients in 2017. Follow up research may benefit from a longer observation period, as well as finer-grained assessment of actual substance use behaviors. Analysis of data of this kind could further assist prevention and intervention efforts.
- For policy makers: Opioid use-related deaths remain a high in the United States. This study indicates that other negative outcomes, such as all-cause mortality and suicidal ideation are also elevated, particularly among patients with opioid and co-occurring substance use disorders. Notably, risk for negative outcomes was highest among those with combined opioid and cocaine use disorder. Enhanced support for research and implementation of prevention and intervention programs could help reduce the likelihood of premature death. Policies and practices at the local and state level around screening for drugs and suicidal ideation could help offset risk as well. In light of publicized cases of drug contamination (e.g., cocaine with fentanyl), campaigns to increase public awareness of these practices and risks might also benefit public health.
CITATIONS
O’Brien, P., Henke, R. M., Schaefer, M. B., Lin, J., & Creedon, T. B. (2021). Adverse events among adult Medicaid enrollees with opioid use disorder and co-occurring substance use disorders. Drug and Alcohol Dependence, 221, 108555. DOI: 10.1016/j.drugalcdep.2021.108555

