Does Exercise Reduce Symptoms of Depression in Former Methamphetamine Users?
Early recovery, a period marked by high risk of relapse, is a vulnerable time for individuals recovering from addiction.
During active addiction, patients often feel compelled to continue using substances in order to experience normal levels of reward due to neuronal receptor down-regulation as the brain adapts to the presence of the drug (a process known as neurobiological neuroadaptation).
In early recovery (when the drug is no longer present), patients may have difficulty experiencing these normal levels of reward because the brain has not yet had sufficient time to recalibrate, readjust, and upregulate these receptors.
Consequently, this type of depression and negative affect can be quite common and persistent in the early months of recovery.
It is important to intervene early since reducing negative affect may help reduce the risk of relapse and result in better treatment outcomes.
Previous studies showing the benefits of exercise interventions for patients with depression and for those in recovery from substance use disorders (see here), it is important to determine if such an intervention has an impact on depressive symptoms of patients in early recovery from methamphetamine (MA) use specifically.
Haglund and colleagues used data from a randomized controlled trial of 135 adults meeting DSM-IV criteria for methamphetamine (MA) dependence in residential treatment to determine which patient factors predict the most significant decreases in depression. In the original study, patients were randomized to exercise training (n = 69) or health education (n = 66) each for three days a week for one hour. The exercise training consisted of supervised aerobic activity and resistance training individually or in pairs. Health education included topics such as nutrition and health screening recommendations.
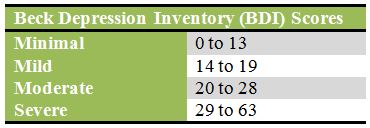
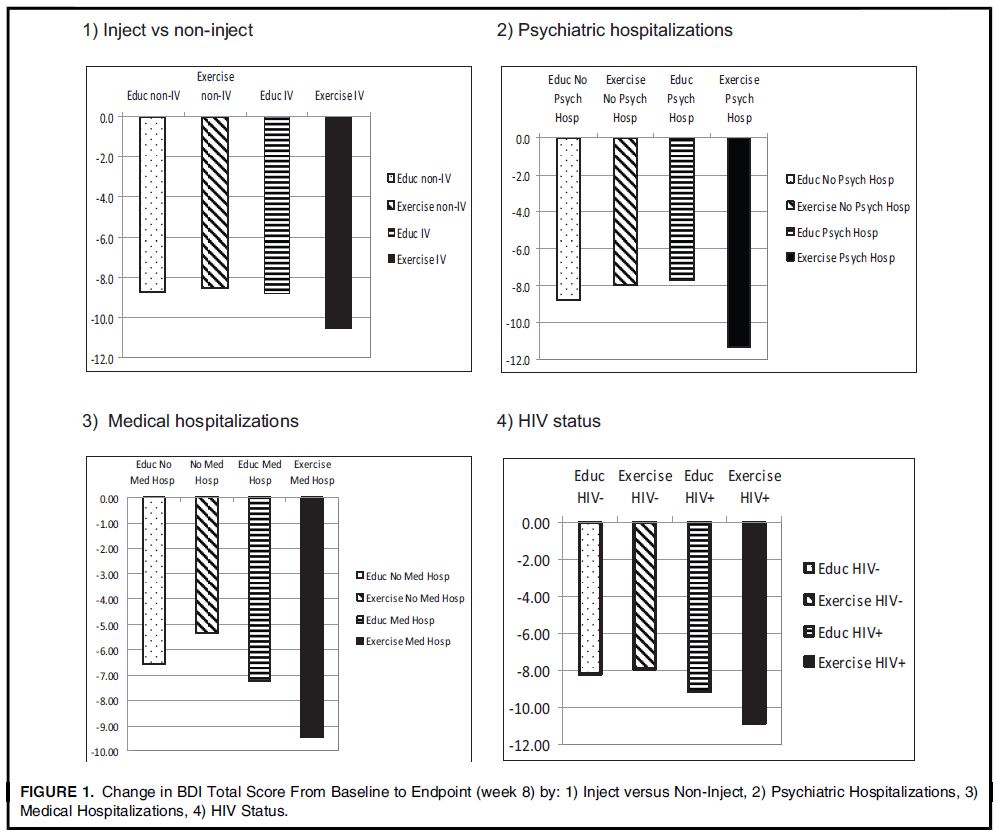
Participants were about 30% female, 84% unemployed, had an average of 12 years of education, and were 32 years old on average. Methamphetamine (MA) use in the month prior to study enrollment was about 16 days on average. There were no differences in baseline characteristics between groups. When examining predictors of depression in both treatment groups, the authors found that individuals who injected MA, had been hospitalized for psychiatric reasons in the past 12 months, had been hospitalized for medical reasons in the past 12 months, and HIV positive individuals experienced significantly greater decreases in Beck Depression Inventory (BDI) than their counterparts. For example, those who injected MA experienced a decrease in BDI of 10.59 points versus 8.54 for those who did not inject.
There were no baseline differences in Beck Depression Inventory (BDI) by group (13.7 for the exercise group versus 12.0 for the education group). By the end of the 8-week study, patients in the exercise group reported a significantly lower BDI score than those in the education group.
The authors also examined predictors of depression among exercise group participants finding largest reductions in Beck Depression Inventory (BDI) among those who injected methamphetamine (MA), had worse medical and psychiatric conditions at baseline (measured by past 12 month hospitalizations), and HIV positive individuals.
Source: (Haglund et al., 2015)
Source: (Eack et al. 2015)
IN CONTEXT
When examining predictors of lowering depression in MA users in residential treatment, the authors of this study concluded that individuals with more severe addiction (i.e., injected methamphetamine (MA)) and poorer medical and psychiatric health at baseline achieved the greatest benefit from this exercise intervention
Treating co-occurring depression among people in early recovery is a priority as depression may undermine progress made during treatment; implementing an exercise intervention with numerous physical and emotional benefits may be an inexpensive solution to this problem.
- LIMITATIONS
-
- This sample included methamphetamine (MA) users in residential treatment so it is not certain that results can be generalized to other MA using populations such as non-treatment seekers and those in outpatient care.
- The residential setting helped facilitate this exercise program so it may be difficult to implement an intervention of the same intensity and frequency in an outpatient treatment center. People in residential treatment are a captive audience so this may be an ideal setting to help patients develop good exercise and other healthy habits. However, it is unknown if the benefits of exercise persist if a patient continues to exercise after leaving treatment and if benefits diminish after a patient stops exercising.
BOTTOM LINE
- For individuals & families seeking recovery: Exercise may help alleviate depressive symptoms. While this study focused on methamphetamine (MA) users in early recovery, experience has been shown to be beneficial across different addictions or primary substances and stages of recovery.
- For scientists: It is unknown what “dose” of exercise is needed to provide benefits for depression among methamphetamine (MA) users. Future studies should evaluate various exercise programs to determine if there is an optimal form of the intervention.
- For policy makers: Exercise may be an inexpensive addition to a treatment plan that provides benefits for multiple facets of a patient’s health.
- For treatment professionals and treatment systems: Exercise can compliment a patient’s existing care with little to no side effects. Regardless of addiction severity, they will likely experience benefits in terms of emotional and mental health.
CITATIONS
Haglund, M., Ang, A., Mooney, L., Gonzales, R., Chudzynski, J., Cooper, C. B., . . . Rawson, R. A. (2015). Predictors of depression outcomes among abstinent methamphetamine-dependent individuals exposed to an exercise intervention. Am J Addict, 24(3), 246-251. doi: 10.1111/ajad.12175

