This US study found that smoking has overtaken injection as the route of administration most often involved in drug overdose deaths.
This US study found that smoking has overtaken injection as the route of administration most often involved in drug overdose deaths.
l
Over the last 3 decades, there have been several fluctuations in opioid use patterns and prevalence estimates in the United States. The predominant opioid involved in overdose deaths shifted from prescription opioids in the 1990’s and early 2000’s, to heroin in 2010, and to synthetic opioids like fentanyl in 2013. Recent estimates suggest that about 70% of drug overdose deaths involve synthetic opioids other than methadone, with fentanyl accounting for the majority of these deaths. Since 2015, there has also been a steady increase in deaths involving both fentanyl and stimulants.
Rising rates of heroin and fentanyl use were accompanied by increased rates of injection drug use. More recent data suggests that the most common route of opioid administration may be shifting from injecting to smoking. However, findings have been limited to the west coast of the United States and few have evaluated trends in route of administration for other drugs, like stimulants.
Routes of drug administration have implications for individuals who use drugs, as well as clinical and public health efforts aimed at combating drug overdose. Gaining a better understanding of national overdose patterns, including the most common routes of drug administration contributing to overdose deaths, can ultimately help guide timely harm reduction services and public health initiatives to help address overdose, infectious disease transmission, and other drug-related harms amid the everchanging landscape of drug use in the United States.
Though injection is arguably the riskiest type of drug administration, given its association with heightened risk of overdose and infectious disease transmission, other routes of administration still pose significant risk. Like injecting, smoking results in very rapid absorption of a drug throughout the body, which increases risk of overdose compared to oral ingestion (i.e., swallowing it). This study investigated whether the predominant route of drug administration involved in overdose deaths has changed over time, as well as the impact of geographic region and drug type on overdose trends.
This study was a retrospective analysis of national data from the Centers for Disease Control and Prevention’s (CDC’s) overdose reporting system, in which drug overdose trends in the United States were evaluated over a period of 2 years.
The researchers investigated changes in drug overdose-death prevalence rates between January 2020 and December 2022. Overdose-death prevalence rates were evaluated for changes over time, overall, and according to the route of drug administration involved in each overdose. These rates were then assessed for geographic/region-specific and drug-specific trends.
Deaths were categorized into 4 categories of administration route: 1) injection; 2) smoking; 3) snorting; 4) ingestion (oral). Categories were not mutually-exclusive; a death could involve more than one route of drug use administration. Other routes of administration were considered but not reported given small sample sizes for other various routs of drug use (e.g., transdermal). For the approximately 50% of the drug overdose deaths with no known route of drug administration, they were part of the denominator capturing total overdose deaths in a given time period but were not compared directly to those with a known route of administration. To examine the role of drug type, drugs involved in overdose deaths were categorized into 4 mutually exclusive categories: 1) fentanyl only; 2) stimulants only; 3) both fentanyl and stimulants; 4) other drug (neither fentanyl nor stimulants).
National data were obtained from the CDC’s State Unintentional Drug Overdose Reporting System, which consists of state-level data on unintentional and undetermined-intent drug overdose deaths obtained from death certificates, postmortem toxicology tests, and coroner/medical examiner reports. Drug overdose-death rates were investigated for change over time by examining overdose prevalence in 6-month intervals, with analyses focusing on comparisons between January – June 2020 and July–December 2022. Routes of drug administration were obtained from autopsy data, crime-scene investigation and witness reports.
States were included in analyses if coroner/medical examiner reports and toxicology reports were available for ≥75% of deaths during the 2-year study period (i.e. January 2020–
December 2022). Overall, 28 states were included in analyses and assessed regionally:
1. Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, Pennsylvania, Rhode Island, Vermont
2. Midwest: Illinois, Kansas, Minnesota, Nebraska, Ohio
3. South: Delaware, District of Columbia, Georgia, Kentucky, Maryland, North Carolina, Oklahoma, Virginia, West Virginia
4. West: Alaska, Arizona, Colorado, Oregon, Utah, Washington
A total of 139,740 overdose deaths were identified across the study period and included in analyses.
National overdose death rates increased by 20% between the years 2020 and 2022
Across all U.S. regions, the number of overdose deaths increased from 21,046 deaths during the first 6 months of 2020 to 25,301 deaths during the final 6 months of 2022 (20% increase). Overdose deaths specifically involving fentanyl increased by 8% (from 71% to 77% of all overdose deaths) during the same period.
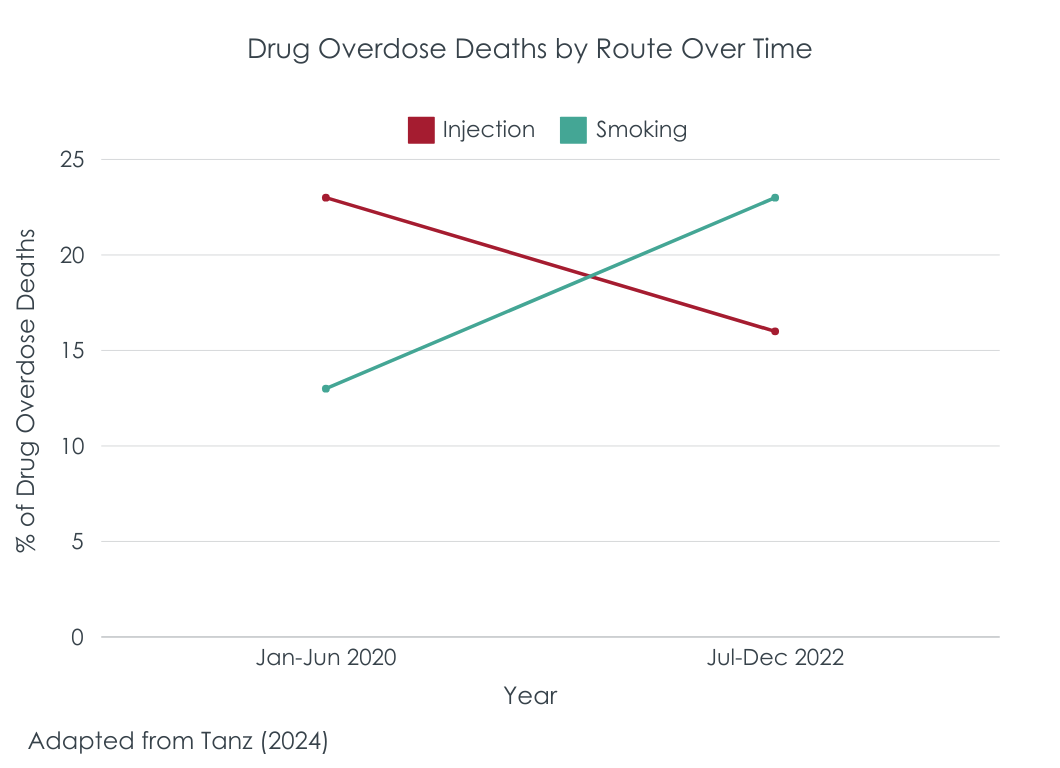
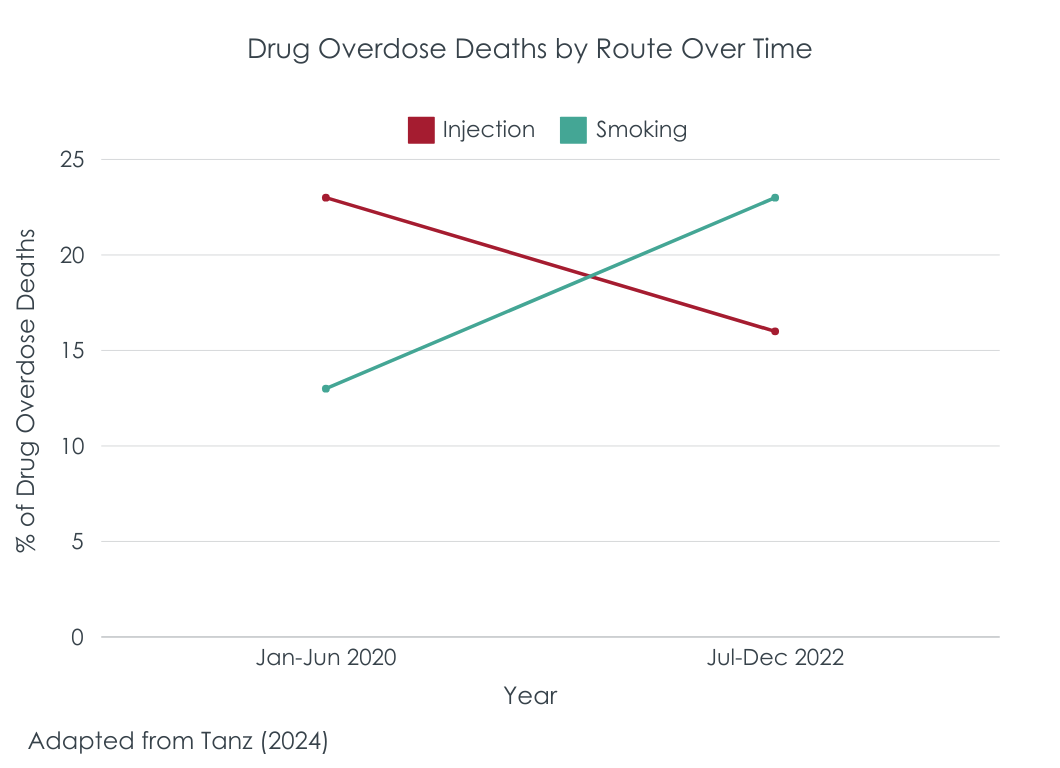
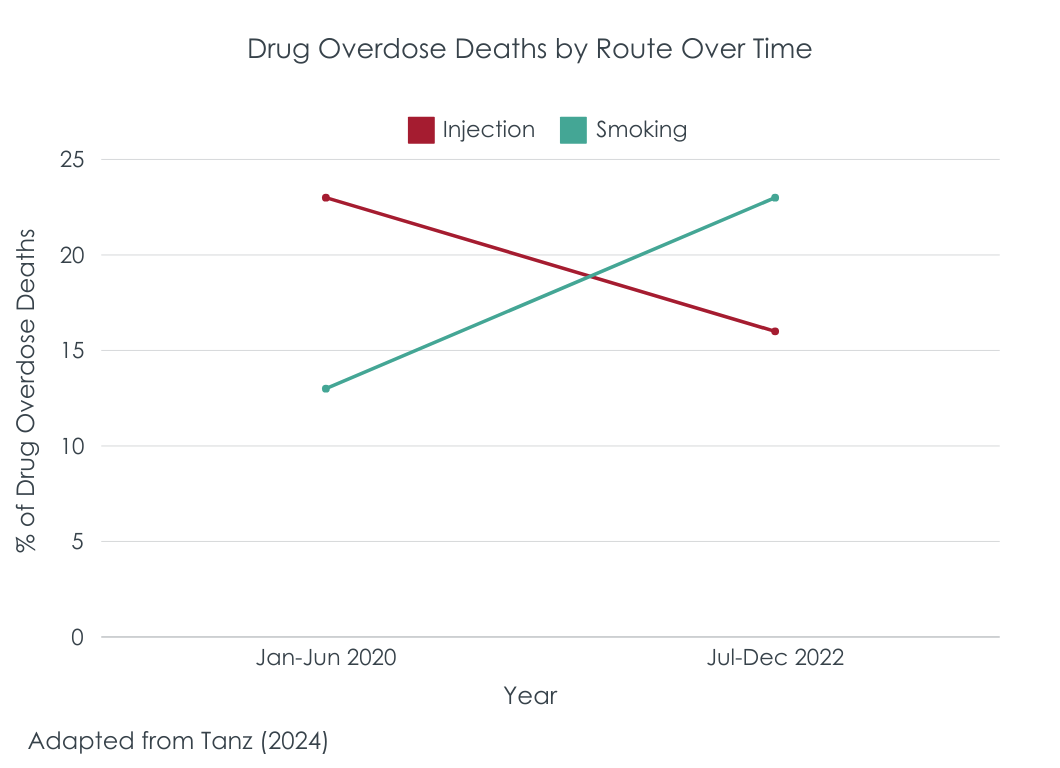
Injection- and ingestion-related drug overdose deaths declined, while smoking- and snorting-related deaths increased
The prevalence of overdose deaths involving injectable and ingestion routes of administration decreased by 29% and 5%, respectively. Conversely, smoking- and snorting-involved drug overdose deaths increased by 74% and 19%, respectively.
The route of administration involved in the greatest proportion of deaths shifted from injection (23% of deaths) in 2020 to smoking (23% of deaths) in 2022. The majority of smoking-, snorting-, and ingestion-involved deaths in 2022 (80%–86%) did not have injection noted as an additional route of administration used at the time of death.
Changes in route-specific overdose death rates were similar across geographic regions
Smoking-involved deaths increased in all U.S. regions and snorting-involved deaths increased in all regions except the West. Injection-related deaths decreased in all geographic regions. In 2022, smoking-involved deaths were the most common type of overdose deaths in the Midwest and West, while both smoking- and injection-involved deaths were most common in the Northeast and South.
Injection-related overdoses decreased, and smoking-related overdoses increased across almost all drug types
Of the overdose deaths in 2020 to 2022, 10%, 6%, 43%, and 8% involved fentanyl only, stimulants only, both fentanyl and stimulants, and neither fentanyl nor stimulants, respectively.
Between the first 6 months of 2020 and last 6 months of 2022, injection-related deaths decreased for overdoses that involved all drug types, including fentanyl alone (42% decrease), stimulants alone (23% decrease), their combination (26% decrease), and drugs other than fentanyl and stimulants (42%).
Smoking-related deaths increased for overdoses that involved fentanyl alone (79% increase), stimulants alone (30% increase), and their combination (65% increase). For overdoses that involved neither fentanyl nor stimulants, smoking-related death rates did not change over time – the most common drug-use route involved in these non-opioid and non-stimulant deaths was oral ingestion throughout the study period.
CDC data showed that smoking-involved drug overdose deaths nearly doubled between 2020 and 2022, with rising death rates observed across all regions of the United States. At the same time, the prevalence of injection-involved drug overdose deaths decreased, and these decreases in injection deaths were greatest for fentanyl-involved deaths. Findings highlighted fentanyl’s ongoing impact on the overdose epidemic, with more recent shifts in the way that people are using fentanyl, with smoking being the most prominent route of administration involved in drug-related deaths in 2022.
The reasons for these shifts in drug-related deaths are not entirely clear. Findings may be partially attributable to the rise of counterfeit pills in the illegal drug supply in recent years. Counterfeit pills often look like legitimate drugs made by pharmaceutical companies (e.g., prescription opioids or benzodiazepines), but these drugs often unknowingly contain fentanyl which poses significant risk for unintentional overdose. Moreover, counterfeit pills are often smoked as opposed to ingested, further increasing one’s risk of overdose. The risks associated with counterfeit pills are evident in drug overdose death rates, with deaths involving counterfeit pills doubling between 2019 and 2021. Other non-pharmaceutical drugs (e.g., methamphetamine) are also commonly cut or contaminated with fentanyl and/or other sedatives (e.g., xylazine), unbeknownst to the person using the drug, again increasing overdose risk.
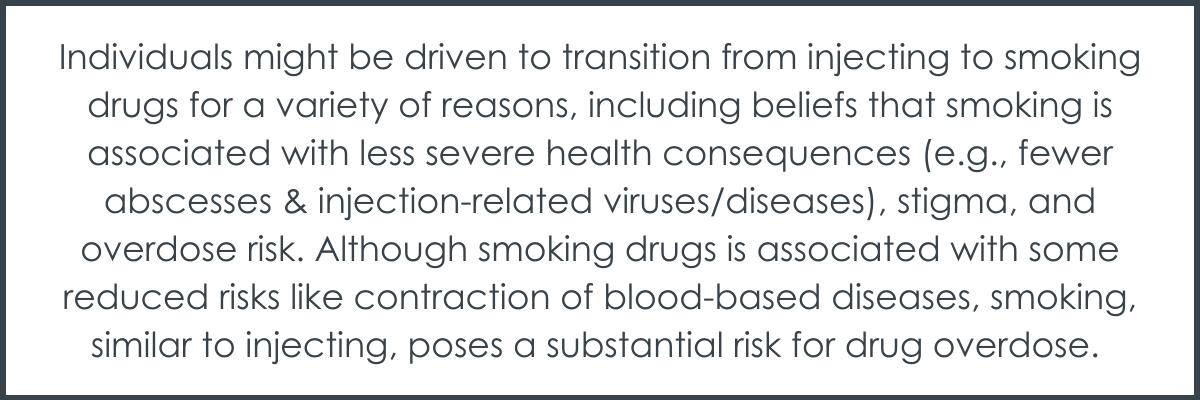
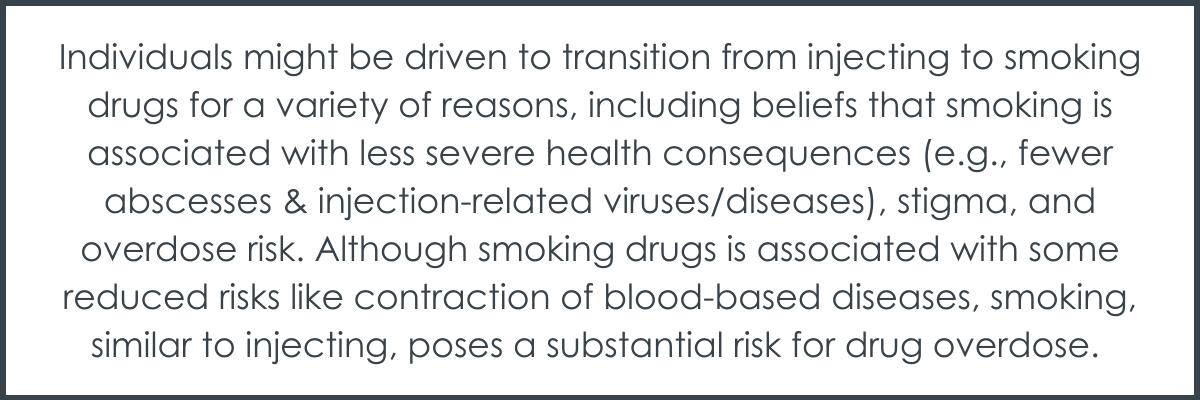
Increased prevalence of smoking-related deaths, and decreased prevalence in injection-involved overdose deaths across all drug classes and geographic regions, might also reflect changing trends in drug-use culture. Recent emphasis on overdose education and public health efforts (e.g., expanding access to naloxone, treatment, and education) aimed at mitigating injection-related harms and overdoses may have encouraged individuals to engage in non-injection routes of drug administration to avoid these harms, thereby reducing the overall number of people experiencing injection-related deaths. Individuals might be driven to transition from injecting to smoking drugs for a variety of reasons, including beliefs that smoking is associated with less severe health consequences (e.g., fewer abscesses & injection-related viruses/diseases), stigma, and overdose risk. Although smoking drugs is associated with some reduced risks like contraction of blood-based diseases, smoking, similar to injecting, poses a substantial risk for drug overdose.
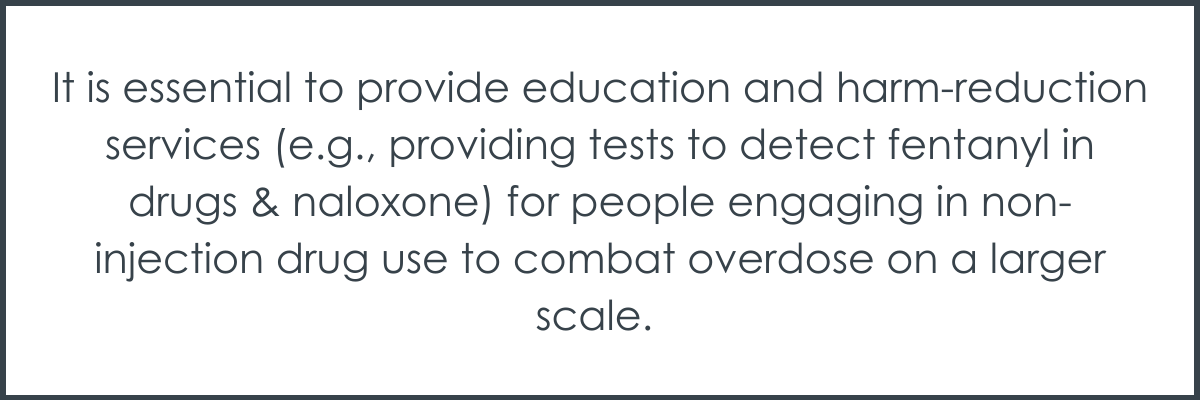
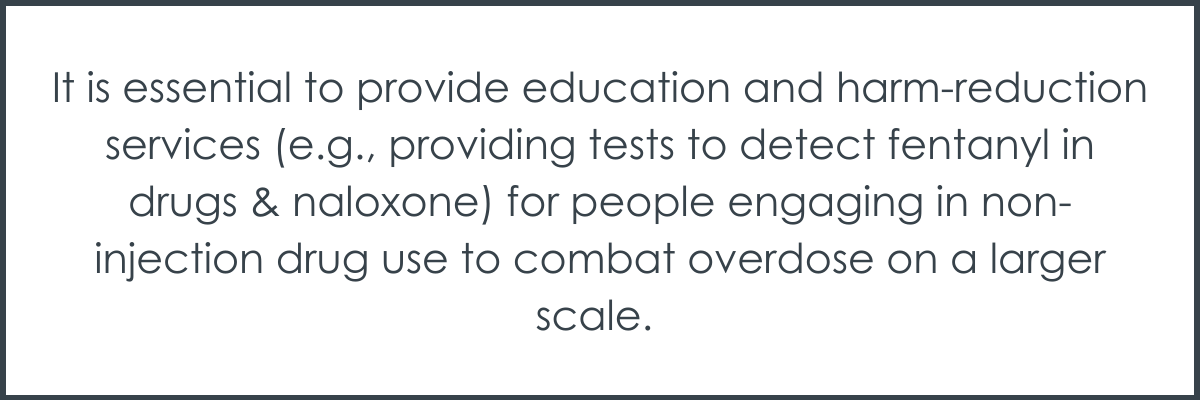
Given that the large majority of overdose deaths that involved smoking, snorting, or ingesting did not also involve injection, it is essential to provide education and harm-reduction services (e.g., providing tests to detect fentanyl in drugs & naloxone) for people engaging in non-injection drug use to combat overdose on a larger scale. People who use drugs but don’t have any experience with injecting may not have access to harm-reduction education and tools because these are often provided in the context of traditional harm-reduction settings like needle exchange programs, which are primarily directed toward individuals who inject drugs.
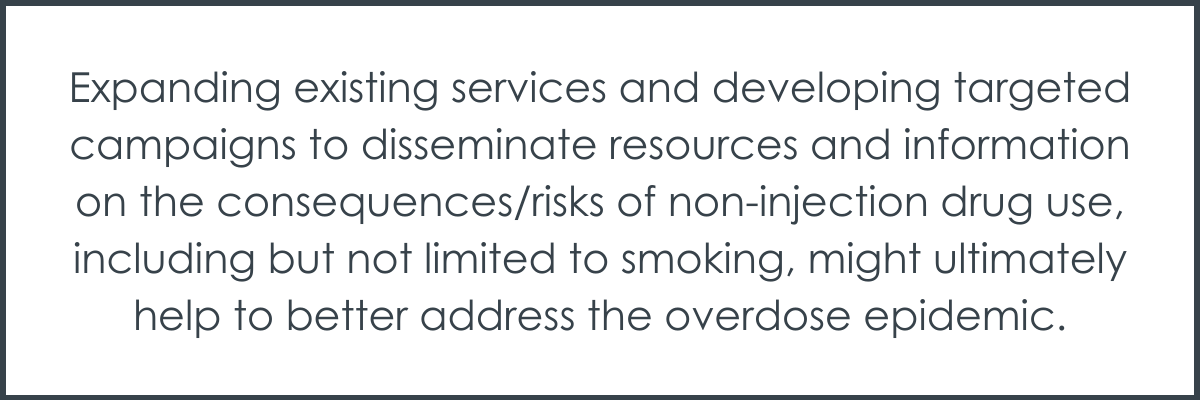
Expanding existing services and developing targeted campaigns to disseminate resources and information on the consequences/risks of non-injection drug use, including but not limited to smoking, might ultimately help to better address the overdose epidemic. Some states have already begun to address these issues by adapting harm reduction services and developing healthcare sites targeting individuals who engage in non-injection drug use to provide safer smoking supplies and associated healthcare. Additional research examining overdose deaths beyond 2022 will help determine whether trends in overdose death rates and associated route of drug administration have changed since the recent introduction of xylazine (a sedative drug) as a new and dangerous contaminant in today’s drug supply.
There has been a shift in drug-overdose death trends in recent years, with injection-related deaths decreasing and smoking-related deaths increasing. Smoking was the most prominent route of administration involved in drug-related deaths in 2022. These shifts in drug-route trends were most robust for fentanyl-involved deaths and were generally consistent across all U.S. regions. The large majority of overdose deaths that involved smoking, snorting, or ingesting did not also involve injection. Thus, this study highlights the public health benefits of expanding education and harm-reduction services to people engaging in non-injection drug use to combat overdose on a larger scale.
Tanz, L. J. (2024). Routes of Drug Use Among Drug Overdose Deaths—United States, 2020–2022. MMWR. Morbidity and Mortality Weekly Report, 73. doi: 10.15585/mmwr.mm7306a2
l
Over the last 3 decades, there have been several fluctuations in opioid use patterns and prevalence estimates in the United States. The predominant opioid involved in overdose deaths shifted from prescription opioids in the 1990’s and early 2000’s, to heroin in 2010, and to synthetic opioids like fentanyl in 2013. Recent estimates suggest that about 70% of drug overdose deaths involve synthetic opioids other than methadone, with fentanyl accounting for the majority of these deaths. Since 2015, there has also been a steady increase in deaths involving both fentanyl and stimulants.
Rising rates of heroin and fentanyl use were accompanied by increased rates of injection drug use. More recent data suggests that the most common route of opioid administration may be shifting from injecting to smoking. However, findings have been limited to the west coast of the United States and few have evaluated trends in route of administration for other drugs, like stimulants.
Routes of drug administration have implications for individuals who use drugs, as well as clinical and public health efforts aimed at combating drug overdose. Gaining a better understanding of national overdose patterns, including the most common routes of drug administration contributing to overdose deaths, can ultimately help guide timely harm reduction services and public health initiatives to help address overdose, infectious disease transmission, and other drug-related harms amid the everchanging landscape of drug use in the United States.
Though injection is arguably the riskiest type of drug administration, given its association with heightened risk of overdose and infectious disease transmission, other routes of administration still pose significant risk. Like injecting, smoking results in very rapid absorption of a drug throughout the body, which increases risk of overdose compared to oral ingestion (i.e., swallowing it). This study investigated whether the predominant route of drug administration involved in overdose deaths has changed over time, as well as the impact of geographic region and drug type on overdose trends.
This study was a retrospective analysis of national data from the Centers for Disease Control and Prevention’s (CDC’s) overdose reporting system, in which drug overdose trends in the United States were evaluated over a period of 2 years.
The researchers investigated changes in drug overdose-death prevalence rates between January 2020 and December 2022. Overdose-death prevalence rates were evaluated for changes over time, overall, and according to the route of drug administration involved in each overdose. These rates were then assessed for geographic/region-specific and drug-specific trends.
Deaths were categorized into 4 categories of administration route: 1) injection; 2) smoking; 3) snorting; 4) ingestion (oral). Categories were not mutually-exclusive; a death could involve more than one route of drug use administration. Other routes of administration were considered but not reported given small sample sizes for other various routs of drug use (e.g., transdermal). For the approximately 50% of the drug overdose deaths with no known route of drug administration, they were part of the denominator capturing total overdose deaths in a given time period but were not compared directly to those with a known route of administration. To examine the role of drug type, drugs involved in overdose deaths were categorized into 4 mutually exclusive categories: 1) fentanyl only; 2) stimulants only; 3) both fentanyl and stimulants; 4) other drug (neither fentanyl nor stimulants).
National data were obtained from the CDC’s State Unintentional Drug Overdose Reporting System, which consists of state-level data on unintentional and undetermined-intent drug overdose deaths obtained from death certificates, postmortem toxicology tests, and coroner/medical examiner reports. Drug overdose-death rates were investigated for change over time by examining overdose prevalence in 6-month intervals, with analyses focusing on comparisons between January – June 2020 and July–December 2022. Routes of drug administration were obtained from autopsy data, crime-scene investigation and witness reports.
States were included in analyses if coroner/medical examiner reports and toxicology reports were available for ≥75% of deaths during the 2-year study period (i.e. January 2020–
December 2022). Overall, 28 states were included in analyses and assessed regionally:
1. Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, Pennsylvania, Rhode Island, Vermont
2. Midwest: Illinois, Kansas, Minnesota, Nebraska, Ohio
3. South: Delaware, District of Columbia, Georgia, Kentucky, Maryland, North Carolina, Oklahoma, Virginia, West Virginia
4. West: Alaska, Arizona, Colorado, Oregon, Utah, Washington
A total of 139,740 overdose deaths were identified across the study period and included in analyses.
National overdose death rates increased by 20% between the years 2020 and 2022
Across all U.S. regions, the number of overdose deaths increased from 21,046 deaths during the first 6 months of 2020 to 25,301 deaths during the final 6 months of 2022 (20% increase). Overdose deaths specifically involving fentanyl increased by 8% (from 71% to 77% of all overdose deaths) during the same period.
Injection- and ingestion-related drug overdose deaths declined, while smoking- and snorting-related deaths increased
The prevalence of overdose deaths involving injectable and ingestion routes of administration decreased by 29% and 5%, respectively. Conversely, smoking- and snorting-involved drug overdose deaths increased by 74% and 19%, respectively.
The route of administration involved in the greatest proportion of deaths shifted from injection (23% of deaths) in 2020 to smoking (23% of deaths) in 2022. The majority of smoking-, snorting-, and ingestion-involved deaths in 2022 (80%–86%) did not have injection noted as an additional route of administration used at the time of death.
Changes in route-specific overdose death rates were similar across geographic regions
Smoking-involved deaths increased in all U.S. regions and snorting-involved deaths increased in all regions except the West. Injection-related deaths decreased in all geographic regions. In 2022, smoking-involved deaths were the most common type of overdose deaths in the Midwest and West, while both smoking- and injection-involved deaths were most common in the Northeast and South.
Injection-related overdoses decreased, and smoking-related overdoses increased across almost all drug types
Of the overdose deaths in 2020 to 2022, 10%, 6%, 43%, and 8% involved fentanyl only, stimulants only, both fentanyl and stimulants, and neither fentanyl nor stimulants, respectively.
Between the first 6 months of 2020 and last 6 months of 2022, injection-related deaths decreased for overdoses that involved all drug types, including fentanyl alone (42% decrease), stimulants alone (23% decrease), their combination (26% decrease), and drugs other than fentanyl and stimulants (42%).
Smoking-related deaths increased for overdoses that involved fentanyl alone (79% increase), stimulants alone (30% increase), and their combination (65% increase). For overdoses that involved neither fentanyl nor stimulants, smoking-related death rates did not change over time – the most common drug-use route involved in these non-opioid and non-stimulant deaths was oral ingestion throughout the study period.
CDC data showed that smoking-involved drug overdose deaths nearly doubled between 2020 and 2022, with rising death rates observed across all regions of the United States. At the same time, the prevalence of injection-involved drug overdose deaths decreased, and these decreases in injection deaths were greatest for fentanyl-involved deaths. Findings highlighted fentanyl’s ongoing impact on the overdose epidemic, with more recent shifts in the way that people are using fentanyl, with smoking being the most prominent route of administration involved in drug-related deaths in 2022.
The reasons for these shifts in drug-related deaths are not entirely clear. Findings may be partially attributable to the rise of counterfeit pills in the illegal drug supply in recent years. Counterfeit pills often look like legitimate drugs made by pharmaceutical companies (e.g., prescription opioids or benzodiazepines), but these drugs often unknowingly contain fentanyl which poses significant risk for unintentional overdose. Moreover, counterfeit pills are often smoked as opposed to ingested, further increasing one’s risk of overdose. The risks associated with counterfeit pills are evident in drug overdose death rates, with deaths involving counterfeit pills doubling between 2019 and 2021. Other non-pharmaceutical drugs (e.g., methamphetamine) are also commonly cut or contaminated with fentanyl and/or other sedatives (e.g., xylazine), unbeknownst to the person using the drug, again increasing overdose risk.
Increased prevalence of smoking-related deaths, and decreased prevalence in injection-involved overdose deaths across all drug classes and geographic regions, might also reflect changing trends in drug-use culture. Recent emphasis on overdose education and public health efforts (e.g., expanding access to naloxone, treatment, and education) aimed at mitigating injection-related harms and overdoses may have encouraged individuals to engage in non-injection routes of drug administration to avoid these harms, thereby reducing the overall number of people experiencing injection-related deaths. Individuals might be driven to transition from injecting to smoking drugs for a variety of reasons, including beliefs that smoking is associated with less severe health consequences (e.g., fewer abscesses & injection-related viruses/diseases), stigma, and overdose risk. Although smoking drugs is associated with some reduced risks like contraction of blood-based diseases, smoking, similar to injecting, poses a substantial risk for drug overdose.
Given that the large majority of overdose deaths that involved smoking, snorting, or ingesting did not also involve injection, it is essential to provide education and harm-reduction services (e.g., providing tests to detect fentanyl in drugs & naloxone) for people engaging in non-injection drug use to combat overdose on a larger scale. People who use drugs but don’t have any experience with injecting may not have access to harm-reduction education and tools because these are often provided in the context of traditional harm-reduction settings like needle exchange programs, which are primarily directed toward individuals who inject drugs.
Expanding existing services and developing targeted campaigns to disseminate resources and information on the consequences/risks of non-injection drug use, including but not limited to smoking, might ultimately help to better address the overdose epidemic. Some states have already begun to address these issues by adapting harm reduction services and developing healthcare sites targeting individuals who engage in non-injection drug use to provide safer smoking supplies and associated healthcare. Additional research examining overdose deaths beyond 2022 will help determine whether trends in overdose death rates and associated route of drug administration have changed since the recent introduction of xylazine (a sedative drug) as a new and dangerous contaminant in today’s drug supply.
There has been a shift in drug-overdose death trends in recent years, with injection-related deaths decreasing and smoking-related deaths increasing. Smoking was the most prominent route of administration involved in drug-related deaths in 2022. These shifts in drug-route trends were most robust for fentanyl-involved deaths and were generally consistent across all U.S. regions. The large majority of overdose deaths that involved smoking, snorting, or ingesting did not also involve injection. Thus, this study highlights the public health benefits of expanding education and harm-reduction services to people engaging in non-injection drug use to combat overdose on a larger scale.
Tanz, L. J. (2024). Routes of Drug Use Among Drug Overdose Deaths—United States, 2020–2022. MMWR. Morbidity and Mortality Weekly Report, 73. doi: 10.15585/mmwr.mm7306a2
l
Over the last 3 decades, there have been several fluctuations in opioid use patterns and prevalence estimates in the United States. The predominant opioid involved in overdose deaths shifted from prescription opioids in the 1990’s and early 2000’s, to heroin in 2010, and to synthetic opioids like fentanyl in 2013. Recent estimates suggest that about 70% of drug overdose deaths involve synthetic opioids other than methadone, with fentanyl accounting for the majority of these deaths. Since 2015, there has also been a steady increase in deaths involving both fentanyl and stimulants.
Rising rates of heroin and fentanyl use were accompanied by increased rates of injection drug use. More recent data suggests that the most common route of opioid administration may be shifting from injecting to smoking. However, findings have been limited to the west coast of the United States and few have evaluated trends in route of administration for other drugs, like stimulants.
Routes of drug administration have implications for individuals who use drugs, as well as clinical and public health efforts aimed at combating drug overdose. Gaining a better understanding of national overdose patterns, including the most common routes of drug administration contributing to overdose deaths, can ultimately help guide timely harm reduction services and public health initiatives to help address overdose, infectious disease transmission, and other drug-related harms amid the everchanging landscape of drug use in the United States.
Though injection is arguably the riskiest type of drug administration, given its association with heightened risk of overdose and infectious disease transmission, other routes of administration still pose significant risk. Like injecting, smoking results in very rapid absorption of a drug throughout the body, which increases risk of overdose compared to oral ingestion (i.e., swallowing it). This study investigated whether the predominant route of drug administration involved in overdose deaths has changed over time, as well as the impact of geographic region and drug type on overdose trends.
This study was a retrospective analysis of national data from the Centers for Disease Control and Prevention’s (CDC’s) overdose reporting system, in which drug overdose trends in the United States were evaluated over a period of 2 years.
The researchers investigated changes in drug overdose-death prevalence rates between January 2020 and December 2022. Overdose-death prevalence rates were evaluated for changes over time, overall, and according to the route of drug administration involved in each overdose. These rates were then assessed for geographic/region-specific and drug-specific trends.
Deaths were categorized into 4 categories of administration route: 1) injection; 2) smoking; 3) snorting; 4) ingestion (oral). Categories were not mutually-exclusive; a death could involve more than one route of drug use administration. Other routes of administration were considered but not reported given small sample sizes for other various routs of drug use (e.g., transdermal). For the approximately 50% of the drug overdose deaths with no known route of drug administration, they were part of the denominator capturing total overdose deaths in a given time period but were not compared directly to those with a known route of administration. To examine the role of drug type, drugs involved in overdose deaths were categorized into 4 mutually exclusive categories: 1) fentanyl only; 2) stimulants only; 3) both fentanyl and stimulants; 4) other drug (neither fentanyl nor stimulants).
National data were obtained from the CDC’s State Unintentional Drug Overdose Reporting System, which consists of state-level data on unintentional and undetermined-intent drug overdose deaths obtained from death certificates, postmortem toxicology tests, and coroner/medical examiner reports. Drug overdose-death rates were investigated for change over time by examining overdose prevalence in 6-month intervals, with analyses focusing on comparisons between January – June 2020 and July–December 2022. Routes of drug administration were obtained from autopsy data, crime-scene investigation and witness reports.
States were included in analyses if coroner/medical examiner reports and toxicology reports were available for ≥75% of deaths during the 2-year study period (i.e. January 2020–
December 2022). Overall, 28 states were included in analyses and assessed regionally:
1. Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, Pennsylvania, Rhode Island, Vermont
2. Midwest: Illinois, Kansas, Minnesota, Nebraska, Ohio
3. South: Delaware, District of Columbia, Georgia, Kentucky, Maryland, North Carolina, Oklahoma, Virginia, West Virginia
4. West: Alaska, Arizona, Colorado, Oregon, Utah, Washington
A total of 139,740 overdose deaths were identified across the study period and included in analyses.
National overdose death rates increased by 20% between the years 2020 and 2022
Across all U.S. regions, the number of overdose deaths increased from 21,046 deaths during the first 6 months of 2020 to 25,301 deaths during the final 6 months of 2022 (20% increase). Overdose deaths specifically involving fentanyl increased by 8% (from 71% to 77% of all overdose deaths) during the same period.
Injection- and ingestion-related drug overdose deaths declined, while smoking- and snorting-related deaths increased
The prevalence of overdose deaths involving injectable and ingestion routes of administration decreased by 29% and 5%, respectively. Conversely, smoking- and snorting-involved drug overdose deaths increased by 74% and 19%, respectively.
The route of administration involved in the greatest proportion of deaths shifted from injection (23% of deaths) in 2020 to smoking (23% of deaths) in 2022. The majority of smoking-, snorting-, and ingestion-involved deaths in 2022 (80%–86%) did not have injection noted as an additional route of administration used at the time of death.
Changes in route-specific overdose death rates were similar across geographic regions
Smoking-involved deaths increased in all U.S. regions and snorting-involved deaths increased in all regions except the West. Injection-related deaths decreased in all geographic regions. In 2022, smoking-involved deaths were the most common type of overdose deaths in the Midwest and West, while both smoking- and injection-involved deaths were most common in the Northeast and South.
Injection-related overdoses decreased, and smoking-related overdoses increased across almost all drug types
Of the overdose deaths in 2020 to 2022, 10%, 6%, 43%, and 8% involved fentanyl only, stimulants only, both fentanyl and stimulants, and neither fentanyl nor stimulants, respectively.
Between the first 6 months of 2020 and last 6 months of 2022, injection-related deaths decreased for overdoses that involved all drug types, including fentanyl alone (42% decrease), stimulants alone (23% decrease), their combination (26% decrease), and drugs other than fentanyl and stimulants (42%).
Smoking-related deaths increased for overdoses that involved fentanyl alone (79% increase), stimulants alone (30% increase), and their combination (65% increase). For overdoses that involved neither fentanyl nor stimulants, smoking-related death rates did not change over time – the most common drug-use route involved in these non-opioid and non-stimulant deaths was oral ingestion throughout the study period.
CDC data showed that smoking-involved drug overdose deaths nearly doubled between 2020 and 2022, with rising death rates observed across all regions of the United States. At the same time, the prevalence of injection-involved drug overdose deaths decreased, and these decreases in injection deaths were greatest for fentanyl-involved deaths. Findings highlighted fentanyl’s ongoing impact on the overdose epidemic, with more recent shifts in the way that people are using fentanyl, with smoking being the most prominent route of administration involved in drug-related deaths in 2022.
The reasons for these shifts in drug-related deaths are not entirely clear. Findings may be partially attributable to the rise of counterfeit pills in the illegal drug supply in recent years. Counterfeit pills often look like legitimate drugs made by pharmaceutical companies (e.g., prescription opioids or benzodiazepines), but these drugs often unknowingly contain fentanyl which poses significant risk for unintentional overdose. Moreover, counterfeit pills are often smoked as opposed to ingested, further increasing one’s risk of overdose. The risks associated with counterfeit pills are evident in drug overdose death rates, with deaths involving counterfeit pills doubling between 2019 and 2021. Other non-pharmaceutical drugs (e.g., methamphetamine) are also commonly cut or contaminated with fentanyl and/or other sedatives (e.g., xylazine), unbeknownst to the person using the drug, again increasing overdose risk.
Increased prevalence of smoking-related deaths, and decreased prevalence in injection-involved overdose deaths across all drug classes and geographic regions, might also reflect changing trends in drug-use culture. Recent emphasis on overdose education and public health efforts (e.g., expanding access to naloxone, treatment, and education) aimed at mitigating injection-related harms and overdoses may have encouraged individuals to engage in non-injection routes of drug administration to avoid these harms, thereby reducing the overall number of people experiencing injection-related deaths. Individuals might be driven to transition from injecting to smoking drugs for a variety of reasons, including beliefs that smoking is associated with less severe health consequences (e.g., fewer abscesses & injection-related viruses/diseases), stigma, and overdose risk. Although smoking drugs is associated with some reduced risks like contraction of blood-based diseases, smoking, similar to injecting, poses a substantial risk for drug overdose.
Given that the large majority of overdose deaths that involved smoking, snorting, or ingesting did not also involve injection, it is essential to provide education and harm-reduction services (e.g., providing tests to detect fentanyl in drugs & naloxone) for people engaging in non-injection drug use to combat overdose on a larger scale. People who use drugs but don’t have any experience with injecting may not have access to harm-reduction education and tools because these are often provided in the context of traditional harm-reduction settings like needle exchange programs, which are primarily directed toward individuals who inject drugs.
Expanding existing services and developing targeted campaigns to disseminate resources and information on the consequences/risks of non-injection drug use, including but not limited to smoking, might ultimately help to better address the overdose epidemic. Some states have already begun to address these issues by adapting harm reduction services and developing healthcare sites targeting individuals who engage in non-injection drug use to provide safer smoking supplies and associated healthcare. Additional research examining overdose deaths beyond 2022 will help determine whether trends in overdose death rates and associated route of drug administration have changed since the recent introduction of xylazine (a sedative drug) as a new and dangerous contaminant in today’s drug supply.
There has been a shift in drug-overdose death trends in recent years, with injection-related deaths decreasing and smoking-related deaths increasing. Smoking was the most prominent route of administration involved in drug-related deaths in 2022. These shifts in drug-route trends were most robust for fentanyl-involved deaths and were generally consistent across all U.S. regions. The large majority of overdose deaths that involved smoking, snorting, or ingesting did not also involve injection. Thus, this study highlights the public health benefits of expanding education and harm-reduction services to people engaging in non-injection drug use to combat overdose on a larger scale.
Tanz, L. J. (2024). Routes of Drug Use Among Drug Overdose Deaths—United States, 2020–2022. MMWR. Morbidity and Mortality Weekly Report, 73. doi: 10.15585/mmwr.mm7306a2