Treatment Utilization for Hazardous Drinking in HIV+ Women
Hazardous alcohol consumption has been frequently reported among women with human immunodeficiency virus (HIV) infection and is associated with negative health effects. Researchers looked at 474 HIV + women with hazardous drinking and found that having social support is associated with an increased likelihood of attending alcohol treatment.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Hazardous drinking is associated with negative health consequences particularly among HIV infected persons. Specifically, hazardous drinking disrupts multiple points on the HIV care continuum such as adherence to medicine (Braithwaite, 2005) and more rapid disease progression. Alcohol treatment services can reduce drinking, however, very little is known about HIV infected women who seek alcohol treatment.
This study aims to identify the factors associated with utilizing alcohol treatment among HIV infected women. By identifying such factors, programs can use targeted interventions to boost alcohol treatment utilization among HIV infected woman.
HOW WAS THIS STUDY CONDUCTED?
This study analyzed data from the Women’s Interagency HIV Study (WIHS), the largest, observational prospective cohort study of women with HIV in the US. The cross-sectional analysis included 474 women who reported hazardous drinking. The researchers sought to identify which factors were associated with increased odds of receiving alcohol treatment (e.g., inpatient, outpatient, Alcoholics Anonymous, halfway houses, etc.) in the past 6 months. The sample is described in terms of alcohol treatment utilization, education, race, and employment status.
WHAT DID THIS STUDY FIND?
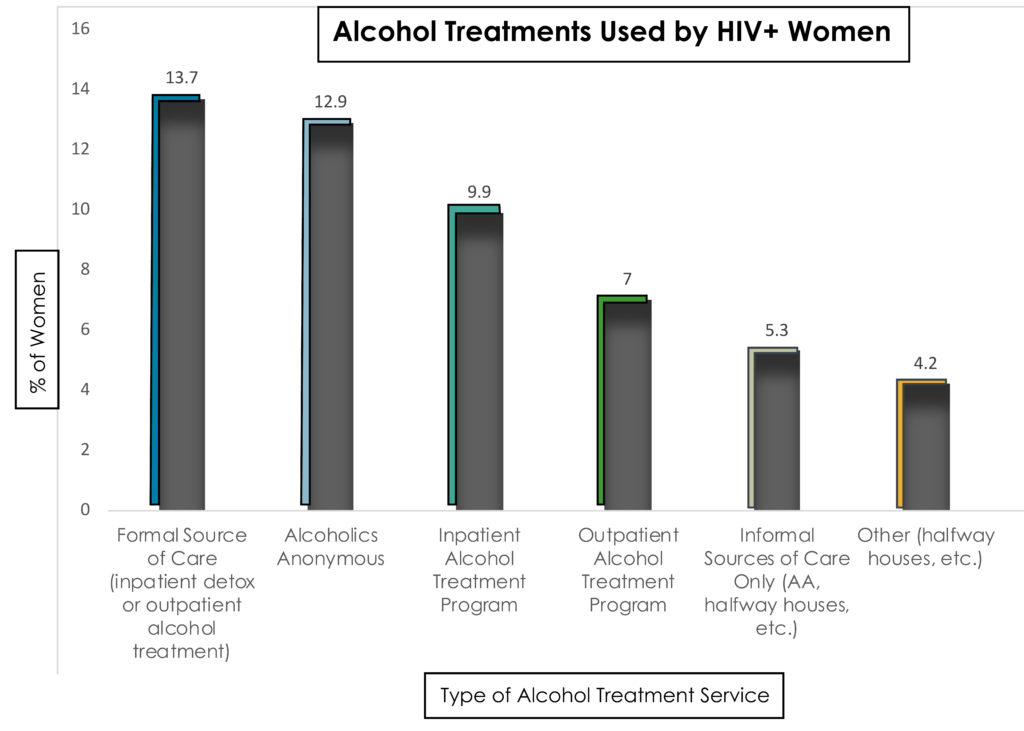
Less than one in five women (19%) reported recent utilization of any alcohol treatment.
Among HIV-positive women with hazardous drinking (≥ 12 drinks per week), alcohol treatment was most often utilized by:
- women who had greater social support
- fewer economic resources
- higher levels of drinking
- reported illicit drug use in the past 6 months.
In the research literature, Alcoholics Anonymous (AA) is generally considered to be a form of peer-led mutual-help (as opposed to treatment by a professional), however, for the sake of analysis this study operationalized AA as a treatment. The sample was primarily Black non-Hispanic (68.6%), had high school or less education (76.8%), and mostly unemployed (85.6%).
WHY IS THIS STUDY IMPORTANT
This study suggests that the availability of auxiliary services, that mimic the benefits of social support (e.g., childcare, transportation, or important family services), may increase alcohol treatment utilization among women with HIV infection.
The utility of offering auxiliary services is further supported by the finding that having fewer economic resources is not uncommon in a population of HIV infected women who seek treatment for hazardous drinking. In addition, providers who treat HIV infected women for alcohol use, should be prepared to address the presence of illicit drug use as well.
- LIMITATIONS
-
- This study was not able to distinguish: 1) women with voluntary versus coerced alcohol treatment utilization; or, 2) women who were unable to get care from women who never sought care. Therefore, we do not know the degree to which greater social support, few economic resources, higher levels of drinking, and use of an illicit drug are equally related to treatment utilization for coerced versus voluntary alcohol treatment or women who are unable to get care versus never sought care. This is an important distinction because when an individual is coerced into treatment, the role of social support or economic circumstances may be less relevant in predicting treatment utilization.
- In addition, due to the cross-sectional design (where participants were only assessed at one point in time), the predictors should not be interpreted as a causal link. For example, because increased social support cannot be established as occurring prior to treatment, it is possible that increased social support occurred as a result of treatment.
NEXT STEPS
Since hazardous drinking and depression frequently co-occur among individuals with HIV infection (Palfai et al., 2014), future research should determine if receiving treatment for depression increases the likelihood of seeking alcohol treatment. In addition, future research should examine differences in drinking and HIV-related health functioning between women who attend treatment versus women who do not.
BOTTOM LINE
- For individuals & families seeking recovery: Seek out friends and family who will provide you with social and emotional support, it may help you get the treatment you need. For families, openly express your emotional support for HIV infected women with heavy alcohol use. Your support may help them overcome social stigma associated with hazardous drinking and HIV and motivate them to seek care for both conditions.
- For Scientists: The results highlighted a profile for HIV infected women who utilized alcohol treatment. The formal diagnoses for alcohol use disorder is lacking. Work needs to be done on how well this profile empirically fits patients with varying levels of alcohol use disorder severity. In addition, the identified predictors are associated with treatment utilization, the relationship to treatment completion or sustained remission is unknown.
- For Policy makers: Vital ancillary services provided by women’s social networks (e.g., childcare, transportation, or important family services) that facilitate access to care, should be considered as a part of the budgetary needs for SUD treatment programs who target HIV-positive women.
- For Treatment professionals and treatment systems: HIV infected women engaging in heavy alcohol use are unlikely to seek help for their alcohol use and may be unaware how alcohol may compromise their HIV-related health conditions as well as other health issues. Determine if their needs often met through social support networks are being addressed (emotional support, help with family care, help with transportation) so barriers to care can be reduced.
CITATIONS
Hu, X., et al., Utilization of Alcohol Treatment Among HIV-Positive Women with Hazardous Drinking, Journal of Substance Abuse Treatment (2016), http://dx.doi.org/10.1016/j.jsat.2016.01.011

