Residential Versus Outpatient Treatment in the US
Residential treatment is associated with increased odds of treatment completion compared to outpatient, but that may not be true for everyone…
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Treatment completion (versus dropout) has been associated with increased odds of abstinence, fewer relapses, higher wages, and less criminal involvement. Outpatient and residential treatment are two of the most frequently used levels of care to treat substance use disorders. There is evidence that treatment completion rates are higher for residential settings. However, this is not always true for everyone; other important factors may also affect treatment completion rates, such as demographics (i.e., age, gender, race-ethnicity) and primary substance (e.g., alcohol, methamphetamine, opioids, etc.).
At the time of this study, little was known about the way treatment settings can interact with both demographic and clinical characteristics to influence the likelihood of treatment completion in a representative U.S. dataset. Ultimately, identifying which treatment settings are best for which patients, may help increase treatment effectiveness to support remission and recovery from substance use disorder.
The purpose of this study was to investigate the relationship between residential versus outpatient treatment and treatment completion, and then to examine how this relationship might vary by demographic characteristics and primary substance.
The researchers hypothesized:
- That the positive impact of residential treatment would differ across age, gender, and racial-ethnic group given that previous research has found that demographic characteristics are associated with the likelihood of treatment completion.
- The association between level of treatment and treatment completion would differ across primary substances and have a stronger relationship with “harder” drugs like cocaine, opioids, and methamphetamine.
HOW WAS THIS STUDY CONDUCTED?
This study used retrospective secondary data analysis from the 2011 Treatment Episode Data Set (TEDS), a federal database of state administrative records on admission and discharge data on substance use disorder treatment that occur in publicly funded facilities. TEDS is considered to cover more than 67% of substance use disorder treatment admissions (public or private) in the U.S.
This analysis included data for first treatment episodes in short-term residential (30 days or fewer) combined with long term residential settings (greater than 30 days), and outpatient treatment only (ambulatory intensive outpatient and non-intensive outpatient). Medical detoxification, opioid agonist treatment (e.g., buprenorphine + naloxone, known by brand name Suboxone), and hospital-based inpatient settings were excluded.
The final sample included 318,924 cases, of which outpatient treatment accounted for 269,783 clients and residential treatment for 49,141 clients. Statistically the researchers ran four separate regression models to test for gender, age, race-ethnicity, and primary substance as a moderating variable. Their primary research question was: Do treatment completion rates for residential and outpatient treatment depend on other factors such a patient’s age, gender, race-ethnicity, or primary substance?
WHAT DID THIS STUDY FIND?
Outpatient treatment accounted for 84.6% of the sample, but had a lower completion rate (51.9%) as compared to residential treatment (64.5%). Clients in residential programs were more than three times as likely to complete treatment as compared to clients in outpatient treatment settings, this effect remained stable even after controlling for many client, clinical, and state level characteristics.
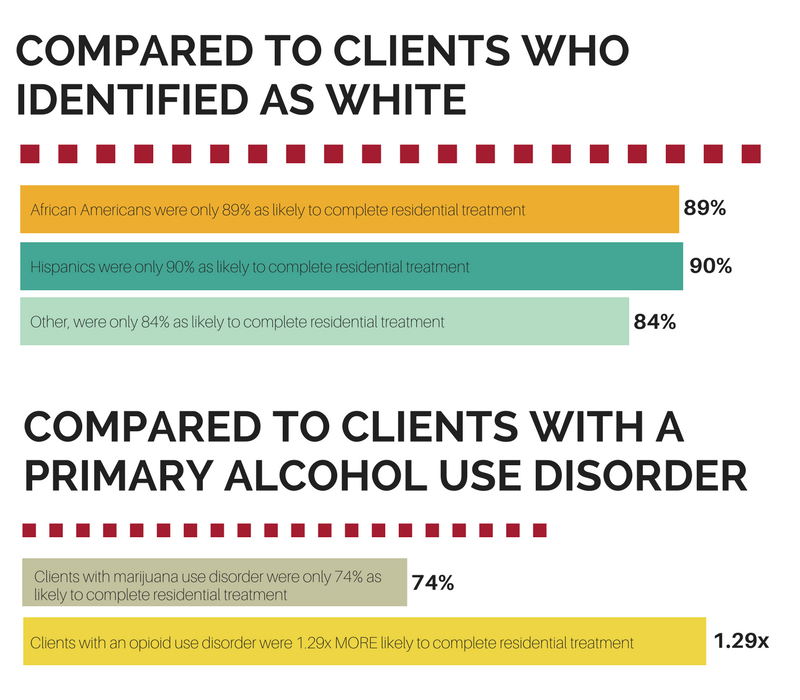
Follow-up analysis revealed that the positive effect of residential treatment on treatment completion was less positive for African Americans and other non-Hispanic clients in long-term treatment only. The positive relationship between treatment completion and short-term residential programs were equivalent across all racial-ethnic groups.
WHY IS THIS STUDY IMPORTANT?
It is important to know which treatment setting will most likely foster treatment completion, remission, and recovery for any given individual. Residential treatment settings generally have higher treatment completion rates than outpatient settings, a finding which was replicated in this study even after controlling for the patients’ clinical or demographic background. Clinical variables included number of substances used and frequency of use; however, number of substance use disorder symptoms as an indicator for severity was not captured.
Patients who identified as White were significantly more likely to complete long-term residential treatment compared to non-White patients. Treatment program differences in factors like cultural competency and cultural communication skills may account for this discrepancy and could also be more important in a residential versus outpatient setting because of the highly structured full time living arrangements required for this level of care.
Patients with a primary opioid use disorder were much more likely to complete treatment in a residential setting compared to those with alcohol use disorder.
The opposite was true for patients with a marijuana use disorder – the degree of benefit offered by residential treatment on treatment completion was less compared to patients with alcohol use disorder. Intensity of cravings and lasting post-acute withdrawal symptoms may play a more substantial role for individuals with an opioid use disorder compared to a marijuana use disorder and the increased structure and clinical oversight provided by residential treatment shields patients from access to opioids while these patients go through the challenging withdrawal and post-acute withdrawal phases of recovery (patients using medications like Suboxone were excluded from this analysis). Given individuals with an opioid use disorder had the lowest completion rates in general, this finding that residential treatment makes a positive difference for treatment completion may be an important way to help this high-risk population.
- LIMITATIONS
-
- Importantly, patients using opioid agonist medication (e.g., methadone or Suboxone) were excluded from the analysis so their potential impact on the results in unknown.
NEXT STEPS
More research needs to incorporate clinical characteristics such as client motivation and therapeutic alliance and the interaction with program factors to better understand who is at risk of drop-out. Research needs to further explore the findings concerning residential treatment being more beneficial for individuals with opioid use disorder compared to alcohol or other drug use disorders.
BOTTOM LINE
- For individuals & families seeking recovery: Treatment for substance use disorder has generally positive effects on reducing substance use and supporting remission. This study found that treatment completion is more likely to be achieved in residential settings compared to outpatient after controlling for many other factors. Furthermore, individuals whose primary substance is opioids are more likely to complete treatment in residential settings compared to outpatient (patients in treatment where medication like Suboxone was the focus were not part of this study, however). Non-White racial-ethnic groups benefited less from a residential setting in terms of treatment completion if enrolled in long-term treatment (but not short-term). If you or a friend have a substance use disorder, it is important to know that treatment completion is associated with less substance use and improved quality of life, so take full advantage of the professional treatment available to you.
- For scientists: Matching treatment to client characteristics, needs, and preferences may improve treatment completion. This study found that patients whose primary substance is opioids are more likely to complete treatment in residential settings compared to outpatient. Yet, treatment non-completion rates for both outpatient and residential are not ideal at about 50% and 65%, respectively. More needs to be done to understand how best to engage patients in treatment so they can complete each phase. Most studies on treatment completion are never able to ask patients about their reasons for dropping out. Whenever possible, qualitative investigations targeting dro-out could prove fruitful for uncovering reasons why non-White racial-ethnic groups in residential settings are less likely to complete long-term treatment given factors that may be explaining the effect of race-ethnicity on outcomes (like level of substance use and criminal justice involvement) are often controlled for in the analysis.
- For policy makers: This national study showed that individuals whose primary substance is opioids are the least likely to complete treatment compared to alcohol or other drugs; however, a residential setting makes a positive difference in terms of treatment completion compared to an outpatient setting. Given the current epidemic of opioid related overdoses in the U.S., this study suggest that greater use of residential treatment should be explored for opioid use disorder in particular. It is not clear from this study, however, how medication access in outpatient treatment settings might change this conclusion. In particular, because this study excluded cases where individuals were in treatment to receive opioid agonist medications like Suboxone, comparisons of those receiving these medications in outpatient setting with those receiving residential treatment are needed to determine whether opioid agonist medication delivered in outpatient settings can mitigate dropout risk for those with opioid use disorder in particular.
- For treatment professionals and treatment systems: Minimizing early drop out and improving the likelihood of treatment completion is an important goal for treatment professionals. Treatment non-completion rates overall remain too high on average nationally. Strategies can be developed and implemented to target the patients most likely to not complete treatment. Greater attention to the factors associated with treatment non-completion is likely to lead to more informed strategies (e.g., targeted use of contingency management) and in turn higher treatment retention and improved outcomes.
CITATIONS
Stahler, G. J., Mennis, J., & DuCette, J. P. (2016). Residential and outpatient treatment completion for substance use disorders in the U.S.: Moderation analysis by demographics and drug of choice. Addictive Behaviors, 58, 129-135.

